
S368
25th European congress of psychiatry / European Psychiatry 41S (2017) S365–S404
EW0759
Decrease in antipsychotic and other
psychotropic medication during 30
months of lifestyle intervention
among outpatients with
schizophrenia
M. Højlund
1 ,∗
, A.F. Elliott
1, N.J. Madsen
1, A.G. Viuff
2, P. Hjort
3,
P. Munk-Jørgensen
41
Aarhus University Hospital Risskov, Department of Affective
Disorders, Risskov, Denmark
2
Regional Psychiatry Services West, OPUS, Herning, Denmark
3
Aarhus University Hospital, Regional Psychiatry Randers, Randers,
Denmark
4
Mental Health Services Region Southern Denmark, Psychiatric
Research Academy, Odense, Denmark
∗
Corresponding author.
Introduction
Patients with schizophrenia have 3-fold higher
mortality from lifestyle diseases, and a long-lasting exposure to
antipsychotic medication may contribute to the development of
somatic illnesses. Region of Central Jutland was inspired by Euro-
pean initiatives to establish a lifestyle intervention program in an
attempt to reduce mortality among individuals with severe mental
illness.
Objectives
To investigate whether this intervention could possi-
bly lower the need for antipsychotic treatment, and to provide a
unique view of actual medication practice.
Aims
To investigate the influence of a lifestyle intervention pro-
gram on changes in antipsychotic medication and polypharmacy in
an unselected cohort of patients with newly diagnosed schizophre-
nia.
Methods
Observational study of outpatients participating in a
programwith individual consultations, group sessions and exercise
groups.
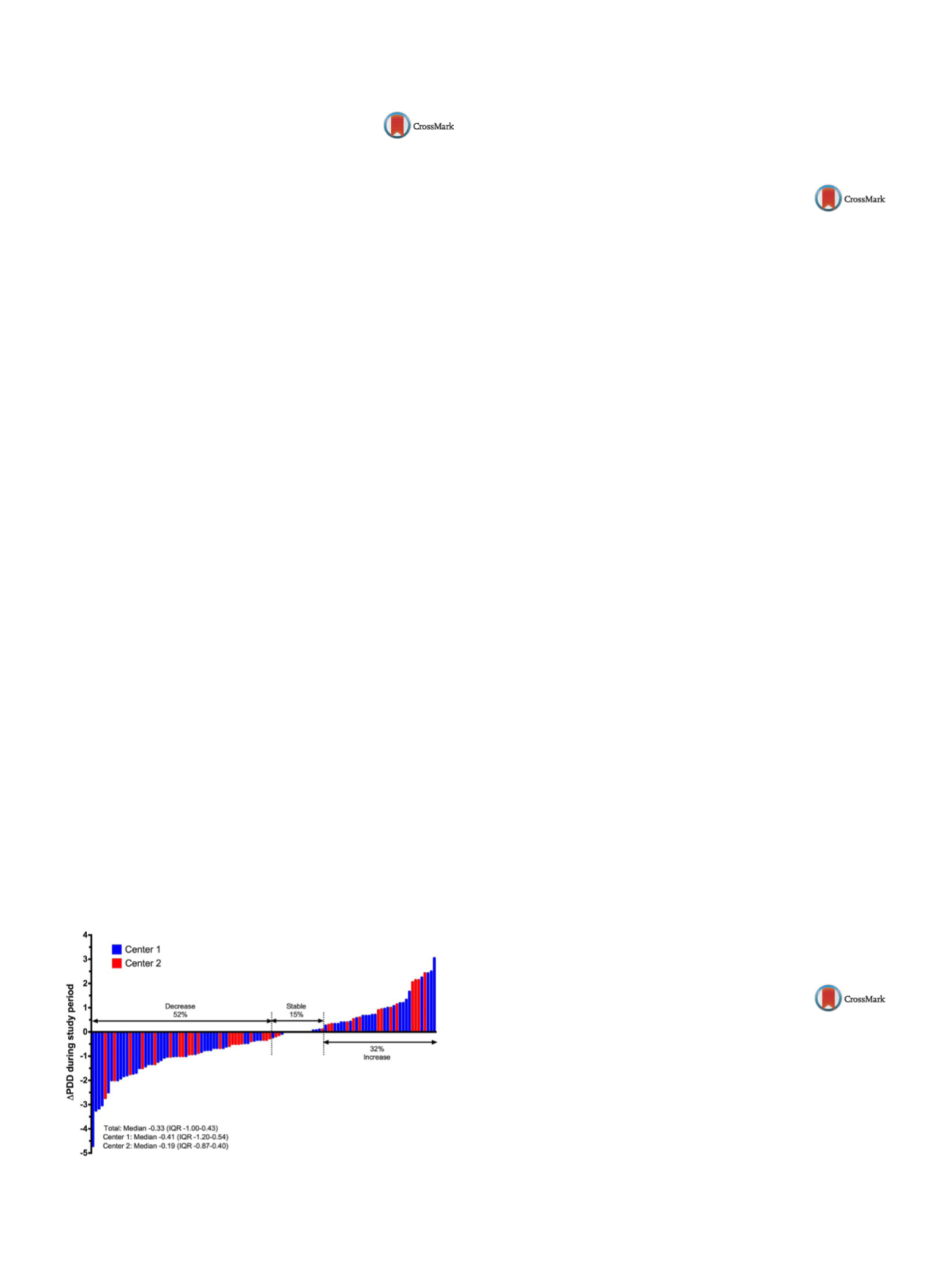
Results
One hundred and eleven patients were eligible for analy-
sis. Fifty-four percent of the patients were subject to antipsychotic
monotherapy. Median Defined Daily Dose (DDD) of antipsychotics
was 1.3 at index (interquartile range [IQR] 0.67–2.00). Fifty-two
percent of the patients experienced a decrease in DDD during the
period with median change of
−
0.33 DDD (IQR
−
1.00 to 0.43). We
found no significant difference in baseline variables or extend of
participation between patients with decrease in doses and patients
with increase
( Fig. 1 ).Conclusions
Most patients decreased or stabilized their doses
of antipsychotic medication during the study period. Half of
the patients were subject to antipsychotic polypharmacy. Extend
and type of participation in the lifestyle intervention pro-
gram did not correlate to changes in dosing of antipsychotic
medication.
Fig. 1
Change in total DDD from index to follow-up (111 patients).
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.373EW0760
Psychiatric comorbidity in patients
affected by fibromyalgia and/or
autoimmune rheumatic diseases:
Preliminary results of an
observational study
A. Bellomo
1, A. Zendoli
1, A. La Marca
1, E. Cuozzo
1,
M. La Montagna
1 ,∗
, A. Rinaldi
1, N. Melillo
2, A. Mele
2,
F.P. Cantatore
21
University of Foggia, Department of Psychiatry, Foggia, Italy
2
Ospedale Riuniti Foggia, Struttura Complessa Reumatologia
Universitaria, Foggia, Italy
∗
Corresponding author.
Introduction
Fibromyalgia is characterized by skeletal muscle
pain and axial stiffness, with elective multiple points of tenderness
(tender points). According to scientific literature, the prevalence of
depression, anxiety and a worse quality of life is higher in patients
with fibromyalgia. Trauma (sexual abuse and physical aggression)
has a key role in the pain perception.
Objectives
To describe the clinical characteristics of patients with
fibromyalgia and/or autoimmune rheumatic diseases admitted to
O.O.R.R. Foggia (Department of Rheumatology), to detect correla-
tion between fibromyalgia and psychiatric disorders.
Aims
To underline psychiatric comorbidity in patients affected
by fibromyalgia and/or autoimmune rheumatic diseases.
Methods
Diagnostic tests at Baseline (T0): Mini International
Neuropsychiatric Interview and Structured Clinical Interview for
DSM Disorder 2 to assess psychopathology, 12-Item Short Form
survey for the quality of life, Diagnostic Criteria for Psychosomatic
Research for disorders of somatic symptoms, Insight Scale for the
awareness of the disease, Davidson Trauma scales to assess the
presence of a post-traumatic stress disorder, Pittsburgh Sleep Qual-
ity Index about the quality of sleep. After 3 months (T1): further
psychodiagnostic assessment for patients with positive mental sta-
tus exam in drug treatment.
Results
Affectivity disorders, feelings of anger, irritability, hostil-
ity, impaired stress response, increased vulnerability to traumatic
events are very frequent in patients affected by fibromyalgia.
Conclusions
The preliminary results of this study show that
patients with fibromyalgia have diagnoses of major depression,
anxiety disorders, post-traumatic stress disorder and personality
disorders (cluster B). Multidisciplinary interventions are needed
integrating the rheumatologic therapy with the psychiatric one,
based on the detected diagnosis.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.374EW0761
Switching to paliperidone palmitate
in an outpatient sample: Preliminary
results of a 43-month follow-up
R. Martín Gutierrez
∗
, R. Medina Blanco , D. Sierra Biddle ,
M.J. Cuesta Nu˜nez , P. Suárez Pinilla
Hospital Universitario Marqués de Valdecilla, Psychiatry, Santander,
Spain
∗
Corresponding author.
Introduction
Patients with psychosis are treated in outpatient
community clinics during most of their lifetime. Antipsychotic
treatments are commonly used in regular clinical practice. How-
ever, the non-adherence is one of the main causes of relapses.


















