
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S583–S644
S607
care services. Piloting this model involves psychosocial rehabilita-
tion of patients with mental disorders, the help of mobile teams at
the place of patient residence, as well as psychoeducation, training,
and support to family doctors. These and other measures will help
to optimise mental health care at PHC level.
Disclosure of interest
The author has not supplied his/her decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.954EV0625
Formative exploration of the
relationship between waiting times
and attendance at general adult
psychiatry clinics, at a hospital in
pennine care NHS Foundation Trust
M. Gani
1 ,∗
, S. Salujha
21
Greater Manchester West Mental Health NHS Foundation Trust,
Chapman Barker Unit- Prestwich Hospital, Manchester, United
Kingdom
2
Pennine Care NHS Foundation Trust, General Adult Psychiatry,
Stepping Hill hospital, Stockport, United Kingdom
∗
Corresponding author.
Introduction
An audit was done to assess new patient wait times.
As part of this project we reviewed possible relationships between
wait times and clinic attendance.
Objective
To examine available data, for possible explanations of
patients’ attendance behaviour at outpatient clinics.
Aims
To identify possible correlation between length of waiting
time for adult psychiatry appointments and status of attendance.
Method
Service Line: New patient referrals to adult outpatient
psychiatry (January–December 2015)
Sample size: 401.
Results
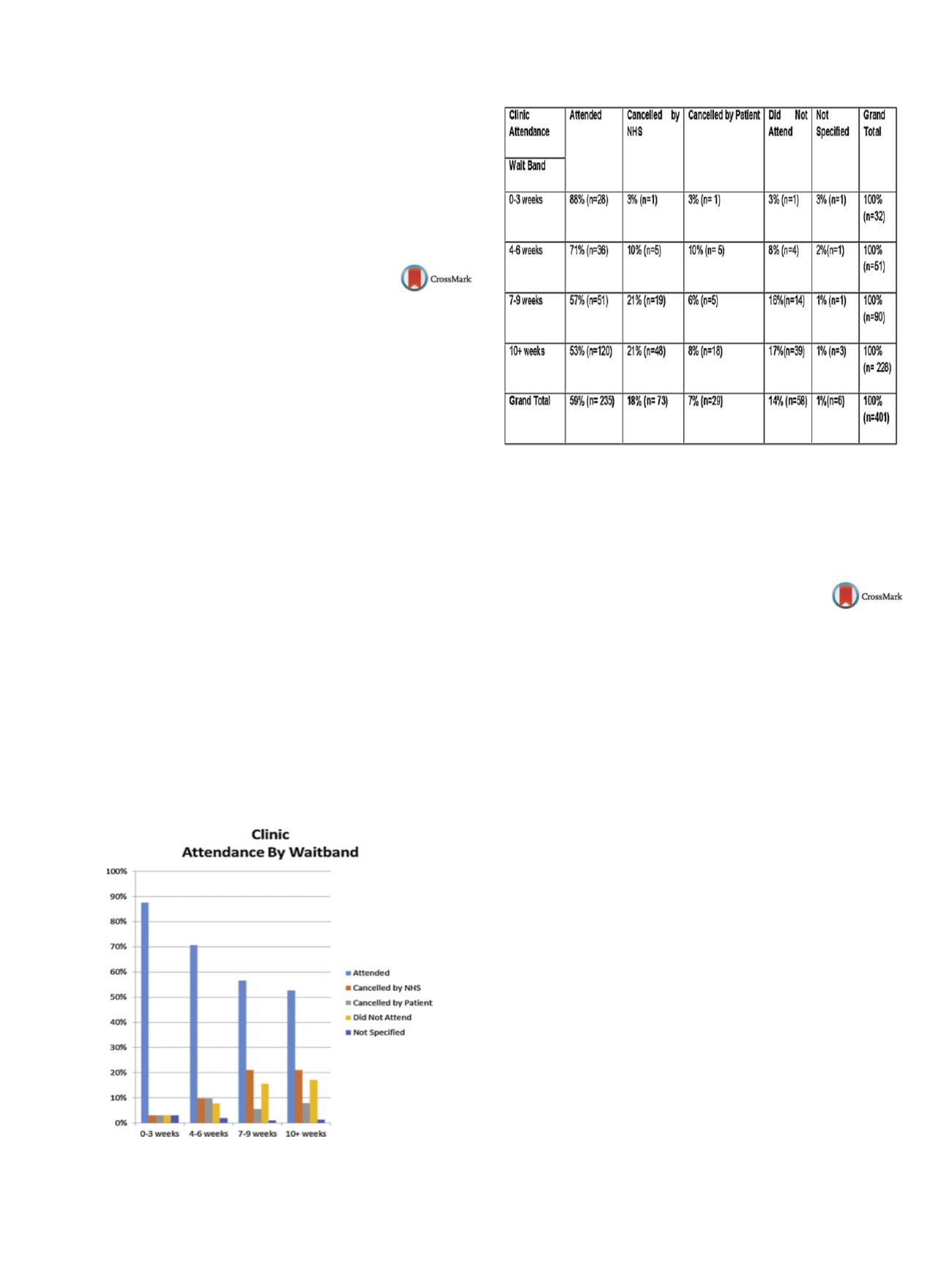
Fig. 1 and
Table 1 show wait times compared with clinic
attendance outcome. Percentage attendance appeared to gradually
fall as wait times increased; while cancellation (%) by the NHS, and
DNAs (did not attend) by the patient, appeared to rise over time.
Conclusions
This review has demonstrated a possible correla-
tion between wait time for a clinic appointment and how patients
behave. The shorter a patient has to wait; it appears they are more
likely to actually attend clinic. If so, this potentially has implica-
tions for discussions around possible reorganization of services, to
improve engagement and outcomes, by coming up with innovative
ways of reducing wait times.
Fig. 1
Clinic attendance by waitband.
Table 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.955EV0626
Descriptive study of adjustment
disorders in a mental health unit.
L. González
∗
, B. Pecino , C. Gomez , M. Anibarro , C. Ortigosa
San Juan Alicante Hospital, Psychiatry, San Juan Alicante, Spain
∗
Corresponding author.
Introduction
Adjustment disorders are a common psychiatric
disorder in primary care and mental health units, with point preva-
lence estimates ranging from 0.9% to 2.3%. These disorders have
been recently defined as a stress response syndrome in the fifth
edition of the DSM, causing emotional and social difficulties and
also a large economic burden on society.
Objectives
The aim of this descriptional study was to analyse the
socio-demographic characteristics and treatment of the patients
diagnosed with adjustment disorders in the first visit in a mental
health unit.
Methods
The study sample consisted of 128 patients admitted for
a psychiatric consultation in amental health unit in Alicante (Spain)
from their primary care physician, between February and July 2016.
Variables of gender, age, current employment status, diagnosis and
treatment were measured. Data analysis was conducted using SPSS
software.
Results
The data from 31 patients who were diagnosed with
adjustment disorders meant a 24% of the sample. The median age
was 47 years old in the adjustment disorders group. Among those
with adjustment disorders, 61% were women, and 52% of them
were unemployed. Almost 60% of themhad at least one pychotropic
prescription and only 22% were derived to psychology.
Conclusions
Adjustment disorders are considered as an interme-
diate category between no mental disorder and affective disorders.
Most authors recommend to start with a psychotherapeutic
intervention. Despite starting with medication has not proved
effectiveness in the studies, most of the patients had at least one
psychotropic prescription before the psychiatric evaluation.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.956

















