
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S521–S582
S565
– coordinating the work of specialists of the local, regional and
federal level;
– interacting with non-governmental organizations;
– setting up a 24-hour “hotline” service (“HL”) on the basis of a
medical institution;
– deploying facilities for providing care to victims, their relatives,
and to “secondary victims”.
Principles of medical-psychological care:
– urgent care must be provided jointly with psychia-
trists/psychotherapists at the places, where the victims are
located;
– individuals with the most severe stress reactions must be identi-
fied and observed by psychiatrists/psychotherapists;
– appropriate and prompt intervention should be made to relieve
acute stress disorders;
– therapeutic interventions should not be a hindrance to victims’
participation in the urgent evacuation and interrogation expedients
as well as completing social tasks.
Disclosure of interest
The author has not supplied his declaration
of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.824EV0495
Anxiety disorder on acting people in
emergencies
S. Oller Canet
1 ,∗
, D. Madariaga Garcia
2, S. Castillo Maga˜na
1,
S. Gasque Llopis
3, V. Adell Anglés
41
Institut de Neuropsiquiatria i Addicions, Centre Emili Mira, Parc de
Salut Mar, Centre de Salut Mental Martí Julià, Santa Coloma de
Gramenet, Spain
2
Parc Sanitari Sant Joan de Déu, Unidad Agudos, Sant Boi de
Llobregat, Spain
3
Institut de Neuropsiquiatria i Addicions- Parc de Salut Mar-, Centre
de Salut Mental La Mina, Barcelona, Spain
4
Parc Sanitari Sant Joan de Déu- Numancia, Unidad de Subagudos,
Barcelona, Spain
∗
Corresponding author.
Introduction
Disasters and emergencies generate a psychological
impact onboth survivors and response teams. Traumatic events and
his memory would be a risk factor for anxiety disorders.
Objectives
Describe the most common post emergency anxiety
signs in a sample of Spanish people who responded directly to
emergencies.
Methods
Study carried out by survey filled through Google Forms
application; in this survey, we retrospectively value anxiety using
the screening scale for generalized anxiety disorder of Carroll and
Davidson.
Results
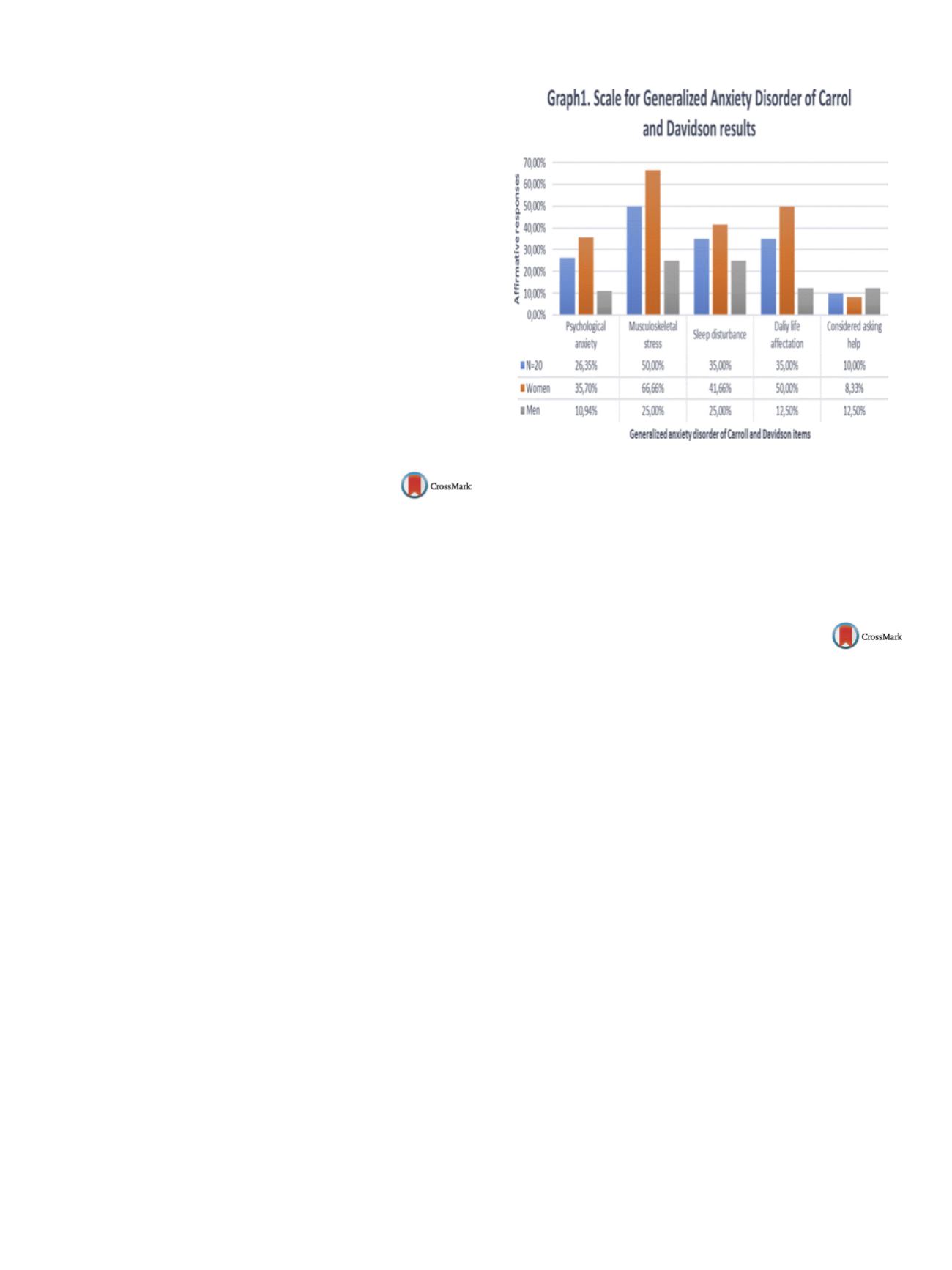
The survey was answered by 20 people, of whom 60%
were women 68.20% age range between 18–6 years and with
university studies in the 70% of the interviewees. Four nurses, 2
doctors, 4 emergency assistantsworkers, 2 civil protectionworkers,
1 ambulance worker, 1 military, 3 policemen, 1 fire-fighter and 2
others. Sixty percent of cases did not received specific aid. The anx-
iety scale items that are most affected are musculoskeletal stress
and sleep, with lower prevalence of psychological anxiety
( Fig. 1 ).Women showed higher prevalence of psychological anxiety, mus-
cle tension, and sleep disturbance.
Conclusions
The data reveals that the staff responding to emer-
gencies recalled experiencedmusculoskeletal problems or sleeping
disturbance better than psychological anxiety which was relegated
to the background. Post-emergency treatment should be provided
to all participants in emergencies including specific interventions
for musculoskeletal stress and insomnia.
Fig. 1
Scale for generalized anxiety disorder of Carrol and David-
son results.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.825EV0496
Change with the times exploring
psychiatric inpatients’ attitudes
towards physical restraint
Y. Spinzy
1 ,∗
, S. Maree
1, A. Segev
2, G. Cohen-Rappaport
11
Shalvata mental health center, A, Tel Vviv, Israel
2
Shalvata mental health center, Emergency, Tel Aviv, Israel
∗
Corresponding author.
Introduction
When other options fail, physical restraint is used in
inpatient psychiatric units as a means to control violent behavior
of agitated inpatients and to prevent them from harm. The profes-
sional and social discourse regarding the use of restrictivemeasures
and the absence of the inpatients’ attitudes towards thesemeasures
is notable. Our research therefore tries to fill this gap by interview-
ing inpatients about these issues.
Objectives and aims
To assess the subjective experience and atti-
tudes of inpatients who have undergone physical restraint.
Methods
Forty inpatients diagnosed with psychiatric disor-
ders were interviewed by way of a structured questionnaire.
Descriptive statistics were conducted via use of SPSS statistical
software.
Results
Inpatients reported that physical restraint evoked an
experience of loneliness (77.5%) and loss of autonomy (82.5%). Staff
visits during times of physical restraint were reported as beneficial
according to 73.6% of the inpatients interviewed. Two thirds of the
inpatients viewed the use of physical restraints as justified when
an inpatient was dangerous. Two thirds of the inpatients regarded
physical restraint as the most aversive experience of their hospi-
talization.
Conclusions
Our pilot study explored the subjective experi-
ence and attitudes of psychiatric inpatients towards the use
of physical restraint. Inpatients viewed physical restraint as a
practice that was sometimes justified but at the same time
evoked negative subjective feelings. We conclude that listening
to inpatients’ perspectives can help caregivers to evaluate these
measures.


















