
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S465–S520
S477
EV0227
Comparative study of psychiatric
comorbidity differences in patients
with ADHD and cocaine substance use
disorders and patients ADHD and
cannabis use disorders
N. Martínez-Luna
1 ,∗
, L. Rodriguez-Cintas
2, C. Daigre
3,
L. Grau-Lopez
4, R.F. Palma-Alvarez
2, A. Esojo
4, C. Roncero
41
Hospital universitario Vall d’Hebron, psychiatry, Barcelona, Spain
2
University hospital Vall d’Hebron, psychiatry- unit of addictions
and dual pathology, Barcelona, Spain
3
University hospital Vall d’Hebron, psychiatry–unit of addictions an
dual pathology, Barcelona, Spain
4
University hospital Vall d’Hebron, psychiatry, Barcelona, Spain
∗
Corresponding author.
Substance Use Disorders (SUD) and Attention Deficit Hyperactive
Disorder (ADHD) are frequent conditions in out drug treatment
centers. There are evidences about the high prevalence of ADHD in
SUDpatients (20%) comparedwith just ADHD in general population
(1–7.3%). Both disorders and psychiatric comorbidity are important
in the diagnosis proceeding. The objective of this study is search the
difference in psychiatric comorbidity conditions between patients
with ADHD and Cocaine SUD and ADHD and Cannabis SUD. ADHD
was present in 158 patients of a total sample in which 46,8% used
cocaine, 17.1% cannabis and 36.1% used both. Mood disorders were
26.8% in cocaine users, 21.7% in cannabis and 18.9% in both. Anxi-
ety disorders were 20.3% in cocaine users, 37.5 in cannabis and 13%
in both users. Primary psychotic disorders were 2.9% in cocaine
users, none in cannabis and 11,1% in both drug users. Personality
disorders by cluster were, Cluster A: 11.3% in cocaine group, 36%
in cannabis group and 24.5 in cannabis and cocaine group. Clus-
ter B: 33.8% in cocaine group, 44% in cannabis group and 51.9%
in cannabis and cocaine group. Cluster C: 9.9% in cocaine group,
28% in cannabis group and 19.2% in cannabis and cocaine group.
There could be common pathways of neuronal damage related to
psychiatric comorbidity depending of used drug, the differences in
comorbidity found in this study could explain a little part of it. It is
important to manage SUD-ADHD and other psychiatric comorbid-
ity in order to improve the outcomes of these patients.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.557EV0228
Gender differences in dual bipolar
disorder
G. Mateu-Codina
1 ,∗
, R. Sauras-Quetcuti
1, A. Farre-Martinez
1,
L. Galindo-Guarín
2, J. Marti-Bonany
2, M.G. Hurtado-Ruiz
3,
M. Campillo-Saenz
3, R. Sanchez-Gonzalez
4,
C. Castillo-Buenaventura
5, M. Torrens-Melich
61
Dual diagnosis unit, institut de neuropsiquiatria i addicions- centre
Emili Mira- Parc de Salut Mar, Santa Coloma de Gramenet Barcelona,
Spain
2
Hospital del Mar medical research institute, IMIM, Barcelona, Spain
3
Acute psychiatric hospitalization program, institut de
neuropsiquiatria i addicions-centre Emili Mira- Parc de Salut Mar,
Santa Coloma de Gramenet Barcelona, Spain
4
CSMA Sant Marti nord, institut de neuropsiquiatria i addicions-
parc de Salut Mar, Barcelona, Spain
5
CAS forum, institut de neuropsiquiatria i addicions- centre fòrum-
parc de Salut Mar, Barcelona, Spain
6
Addiction program, institut de neuropsiquiatria i addicions-
hospital del Mar, Barcelona, Spain
∗
Corresponding author.
Introduction
Women with bipolar disorder are more prone to
psychiatric co-morbidity as anxiety, substance use disorders, eating
disorders and borderline personality disorder. Nevertheless, sub-
stance abuse disorders as co-morbidity in bipolarity are higher in
males than females.
Objectives
To describe differential characteristics of patients
admitted to a psychiatric unit referring to gender in a group of
patientswith bipolar disorder co-morbidwith substances disorders
(dually diagnosed patients).
Methods
Sociodemographic, clinical and administrative data of
all patients diagnosed with bipolar admitted to a dual diagnosis
during a 3-year period were collected. The psychiatric diagnosis
was made according to DSM-IV-R criteria.
Results
From the whole sample (
n
= 66), males (84.8%) were
prevalent. Mean age were 37.71
±
11.7 and mean length of admis-
sion was 24.94
±
17.9 days. Cannabis (34.8%) and cocaine (33.3%)
were the most frequent SUD diagnosis and main reasons for admit-
tance were conduct disorder (33.3%) and mania (25.8%).
Women showed higher length of admission, higher severity scores
at admission and greater reduction in severity scores along hospi-
talisation. No other clinical or sociodemographic differences were
found comparing both groups of patients
( Tables 1–4 ).Conclusions
Women affected by dual bipolar disorder showed
higher severity scores at admission but achieved better remission
rates during hospitalisation.
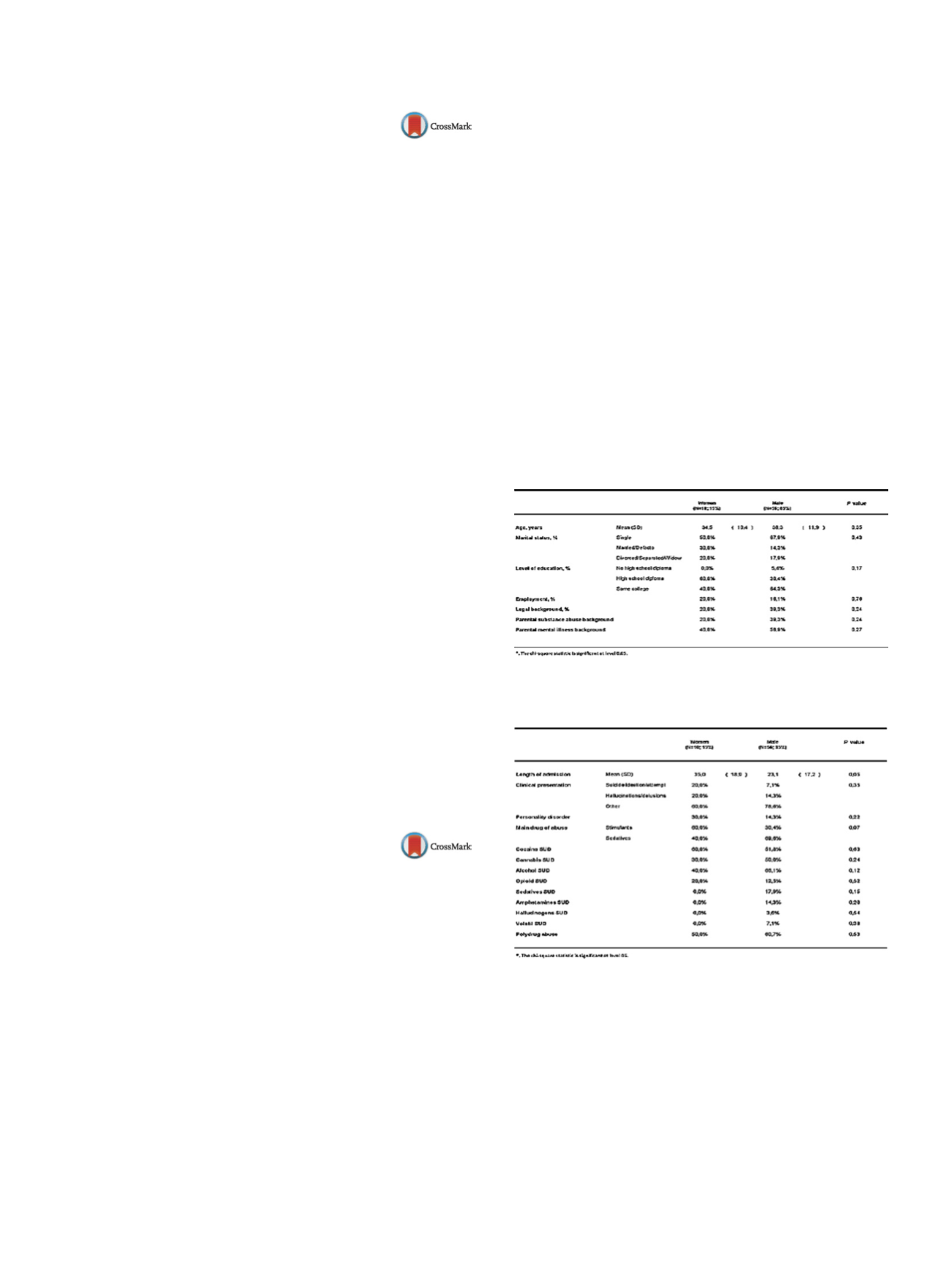
Table 1
Demographic characteristics of both groups.
Table 2
Clinical and functional variables at admission in both
groups.


















