
S478
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S465–S520
Table 3
Historical data about age of drug use in both groups.
Table 4
Severity Scores for both groups of study.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.558EV0229
GERD is associated with the outcome
of MDD treatment
K. Mati´c
1 ,∗
, I. ˇSimunovi´c Filipˇci´c
2, ˇZ. Baji´c
3, I. Filipˇci´c
11
Psychiatric hospital Sveti Ivan, psychiatric hospital Sveti Ivan,
Zagreb, Croatia
2
University hospital center Zagreb, department of psychological
medicine, Zagreb, Croatia
3
Biometrika healthcare research, Zagreb, Croatia
∗
Corresponding author.
Introduction
Gastroesophageal reflux disease (GERD) is more
prevalent among patients with major depressive disorder (MDD)
than in general population, and vice versa. Bidirectional association
of GERD and MDD is well documented. Although protective effect
for gastric symptoms has been indicated for several antidepressants
like trazodone, citalopram, fluoxetine, mirtazapine or fluvoxam-
ine, these findings are sometimes contradictory. Similar may be
claimed for antidepressive effect of some proton pump inhibitors.
We decided to examine the association of GERDwith the long-term
efficacy of MDD treatment.
Objective
To examine the association of GERD and efficacy of
MDD treatment.
Methods
This nested cross-sectional study was done during
2016 at Psychiatric hospital Sveti Ivan, Zagreb, Croatia on the
sample of 1008 psychiatric patients. Key outcome was the number
of psychiatric rehospitalizations since the first diagnosis of MDD.
Predictor was patient-self-declared diagnosis of GERD. Covariates
controlled by multivariate analysis of covariance were sex, age,
duration of MDD in years, education, marital status, number
of household members, work status, clinical global impression
scale–severity of MDD at diagnosis, treatment with tricyclic antide-
pressants (TCA), selective serotonin reuptake inhbitors (SSRI),
serotonin-norephinephrine reuptake inhibitors (SNRI), noradren-
ergic and specific serotonergic (NaSSA) and antipsychotics.
Results
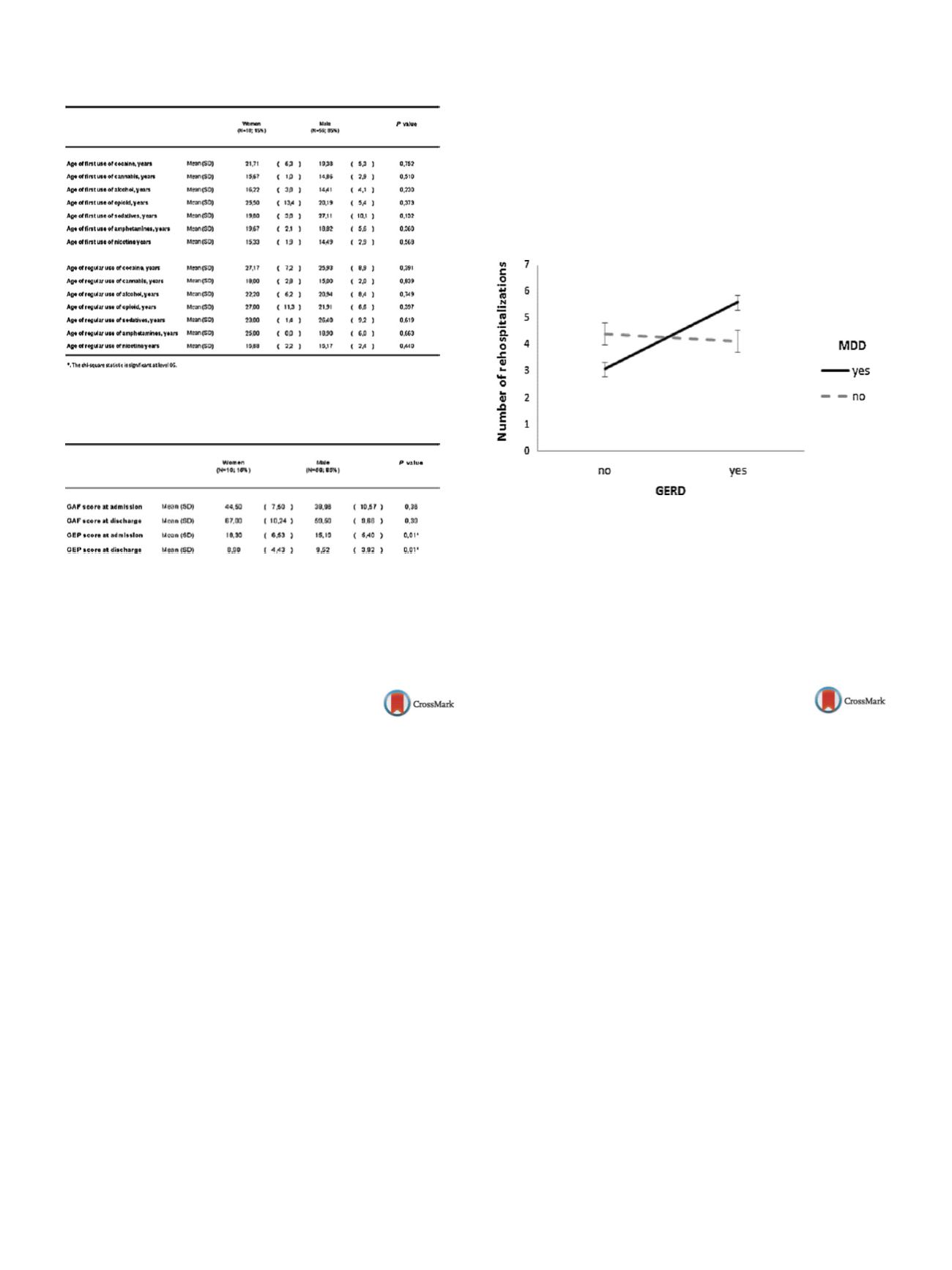
MDD patients with GERD had significantly larger num-
ber of psychiatric rehospitalizations (mean = 5.4 (SD 6.82)) than
MDD patients with no GERD (mean = 3.1 (SD 4.45)). After adjust-
ment for all covariates, GERD significantly moderated the efficacy
of treatment of MDD (
P
= 0.048;
2
= 0.05)
( Figure 1 ).Conclusion
To treat MDD effectively we should treat GERD as
well.
Figure 1
Number of psychiatric rehospitalizations in patients
withMDD and GERD; error bars represent 95% confidence intervals
(
n
= 1008).
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.559EV0230
Comorbidity of major depressive
disorder and personality disorder
increase the risk for suicide
A. Mihai
1 ,∗
, M. Mihai
1, M.S. Mocan
1, C.I. Moga
1, E.V. Nistor
2,
A. Mihai
31
University of medicine and pharmacy “Iuliu Hatieganu”, Student,
Cluj-Napoca, Romania
2
University of medicine and pharmacy, Targu Mures, Student, Targu
Mures, Romania
3
University of medicine and pharmacy, Targu Mures, Psychiatry,
Targu Mures, Romania
∗
Corresponding author.
Introduction
Personality disorder (PD) with an associated diag-
nostic of major depressive disorder (MDD) is a common occurrence,
being considered a factor of treatment resistant depression. In this
study, we compare two groups of patients’ one group having Major
Depressive Episode (MDD) and the other with MDD and PD as
comorbidity.
Methods
This is an observational study of all patients admitted
with diagnosis of MDD during onemonth period in an acute psychi-
atric hospital. Data collection is made using patients files. During
one month period a total number of 105 MDD cases were recorded
(group A-75 cases with MDD and group B-30 patients with PD and
MDD). The diagnosis was recorded in files by a specialist psychia-
trist. Data is analyzed using SPSS v.20.
Results
A significant difference is found when comparing age
groups, mean age for group A being 60 years and for group B
35 years (
P
= 0.05). Regarding suicide attempts a higher prevalence
is found in Group B (Group A 6.7%, Group B 20%) although with
statistical relevance (
P
= 0.04). Study limitation: small sample size
of group B does not allow analysis on different type of personality


















