
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S465–S520
S505
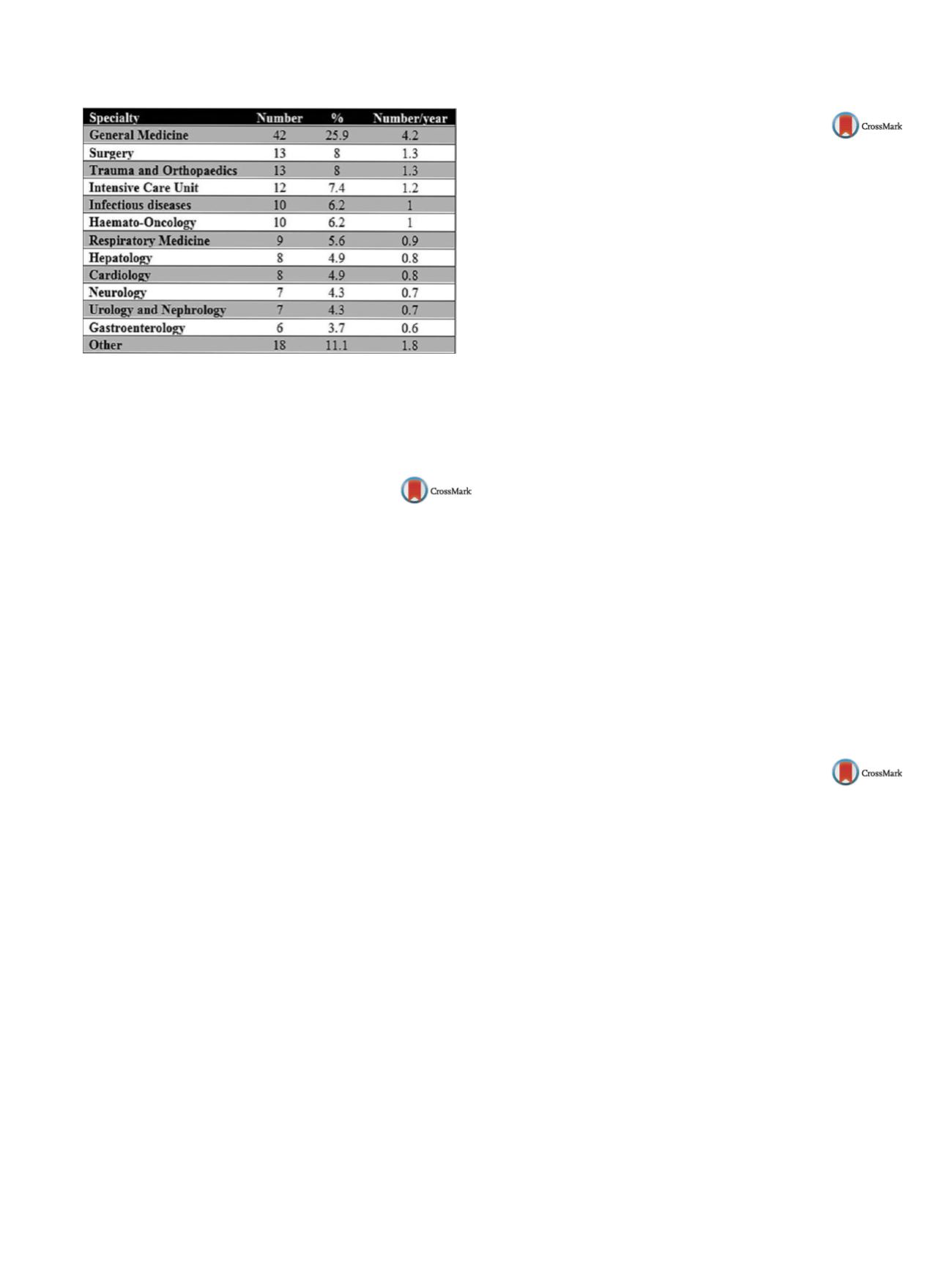
Table 1
Referral source (
n
= 163).
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.639EV0310
A case report of mansonellosis with
neuropsychiatric symptoms
R. Sánchez González
1 ,∗
, D. Maia Asseiceiro
2, R. Torres Miravet
31
Institut de Neuropsiquiatria i Addiccions. Parc de Salut Mar,
department of Psychiatry, Barcelona, Spain
2
Hospital Dos de Maig - CAP La Pau, Family and community
medicine, Barcelona, Spain
3
Hospital Obispo Polanco, department of Psychiatry, Teruel, Spain
∗
Corresponding author.
Introduction
According to the WHO, tropical diseases affect 1/5
of the world population, being increasingly frequent in Europe.
Most of these diseases produce mainly physical symptoms, but the
appearance of accompanying neuropsychiatric symptoms are not
uncommon.
Objective
To present a clinical case of mansonellosis with neu-
ropsychiatric symptoms.
Clinical case
Twenty-two-year-old man from Equatorial Guinea,
resident in the European Union for 3 years without psychiatric
history. His medical history included recurrent malaria, syphilis
treated with penicillin and he was HBsAg carrier.
He presented with a 10month history of headache, pruritus, ret-
rograde amnesia, episodes of anxiety and persecutory delusions.
Previously he had gone to the emergency room several times. Cra-
nial CT scan showed no abnormalities. Anxiolytic treatment with
benzodiazepines was started, with partial response of the symp-
toms.
The blood tests revealed a WBC count of 62
×
10E9/L leukocytes
with 11% eosinophils, IgE 5242 IU/mL and IgG 1740mg/dL. Given
the suspicion of filarial infection, a thick blood film was done,
the result being positive for
mansonella perstans
. He was admin-
istered treatment with albendazole 400mg/12 h for 10 days and
ivermectin in single dose. One month after start of treatment the
patient was asymptomatic with complete resolution of the neu-
ropsychiatric symptoms and correction of eosinophilia.
Results
The patient’s origin, his medical history and the typical
symptoms of parasitosis should raise the suspicion of an infectious
origin of the neuropsychiatric symptoms.
Conclusions
The patients from tropical regions with neurologi-
cal and/or psychiatric symptoms should undergo comprehensive
diagnostic workup to rule out an infectious disease as a possible
cause.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.640EV0311
Describing the assistance, the basis for
improvement
E.J. Pérez Sánchez
∗
, J.M. Ginés Miranda , V. Chavarría Romero ,
J. Moreno , A. Palma , L. Alba Pale , J. Leon , A. Bulbena , V. Perez
Institut de Neuropsiquiatria i Addiccions, Psychiatry, Barcelona, Spain
∗
Corresponding author.
Introduction
Consultation-liaison (CL) psychiatry is a branch of
psychiatry that study and treat mental health of patients with other
medical or surgical conditions. The assistance between hospitals
and health services is heterogeneous.
Aims and objectives
For this reason, the objective of our research
is to define the clinical characteristics fromour CL service and check
out the quality relationship with the applicant service, for improv-
ing future assistance.
Methods
We made a descriptive analysis of clinical variables
from the patients who received assistance during 2months by the
CL service from the hospital del Mar, Barcelona. We got the fre-
quencies and we used the Chi
2
test for the comparison between
variables: Diagnosis, appearance in the report and treatment in the
report.
Results
Total of the sample: 42 patients, 61.9%women. Mean age:
55.1 years. Psychiatric diagnosis was present before the assistance
on 57.1% of the patients. The most frequent diagnosis was Adjust-
ment Disorder (47.6%) and more than one diagnosis was made in
the 14.3%. Near the half of the patients required only primary care
assistance after the discharge from the hospital. In the 68.3% of the
reports appeared information about CL assistance and the indicated
treatment didn’t appear in all the reports. Statistically significant
differences weren’t found in the comparisons.
Conclusions
Adjustment Disorder is supposed to be the most
common psychiatric diagnosis in our CL psychiatry service, as we
found in the reviewed literature. The results reveal that relation-
ships between services can be improved. More studies must be
done for completing information in this issue.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.641EV0312
Neurocognitive profile of patients
with early stages of HIV infection
P. Garcia
1, D. Hernandez
2, C. Fillizola
2, J.M. Santacruz
2,
H. Santamaría García
3 ,∗
1
Pontificia Universidad Javeriana, Psychiatry-Physiology, Bogotá,
Colombia
2
Pontificia Universidad Javeriana, Psychiatry, Bogotá, Colombia
3
Pontificia Universidad Javeriana, Psiquiatría, Bogotá, Colombia
∗
Corresponding author.
HIV-associated neurocognitive disorders (HAND) may include neu-
rological disorders of various severities such as AIDS dementia
complex (ADC) also known as HIV dementia and HIV-associated
dementia (HAD), HIV encephalopathy, and Mild Neurocognitive
Disorder (MND). As it seems HIV-associated neurocognitive dis-
orders are associated with a metabolic encephalopathy induced by
HIV infection and fueled by immune activation of macrophages and
microglia. Despite of a group, evidences have described presence
of cognitive alterations in HIV patients at different stages of HIV
infection so far; little is known about the neurocognitive state of
patients at very early stages of HIV infection. Here, we explored the
neurocognitive profile of a group of cases of HIV patients at very
early stages of HIV infection. We have analyzed of three groups of
subjects, thus, we have studied a group of patients with early HIV
infection, a healthy control group and a group of patients with mild
cognitive impairment due to neurodegenerative causes. Our results
suggested that cognitive processes are sensitive to very early neu-


















