
S760
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S710–S771
they either have a more favorable SD profile. (3) SD with vortiox-
etine was not statistically higher when compared with placebo,
and was statistically lower compared with other SSRIs or SNRIs.
(4) There is evidence that antidepressants that are also 5–HT1A
receptor agonists (e.g. vortioxetine and vilazodone) may facilitate
sexual performance.
Conclusions
In case of SD pharmacologic and non-pharmacologic
options are available. Vortioxetine seems to be a good pharmaco-
logic option, with better NNH than SNRI and less SD.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1425EV1096
Aripiprazole once monthly outpatient
experience
P. Sánchez Páez
∗
, J.L. Gómez Cano , L. Sánchez Flores ,
R. González Lucas , P. Artieda Urrutia
Hospital Ramón y Cajal, Psychiatry, Madrid, Spain
∗
Corresponding author.
Introduction
Aripiprazole oncemonthly (AOM) is one of themost
recently introduced antipsychotics with a different mechanism of
action, which seems to bring clinical and tolerability implications
[1] .Objectives
We describe the patient profile that may benefit from
AOM treatment.
Methods
This is a single-centre, retrospective, one year follow-
up study of 13 cases of ambulatory AOM use. We analyze clinical
and functional evolution, and the tolerability profile of patients in
a real clinical practice basis.
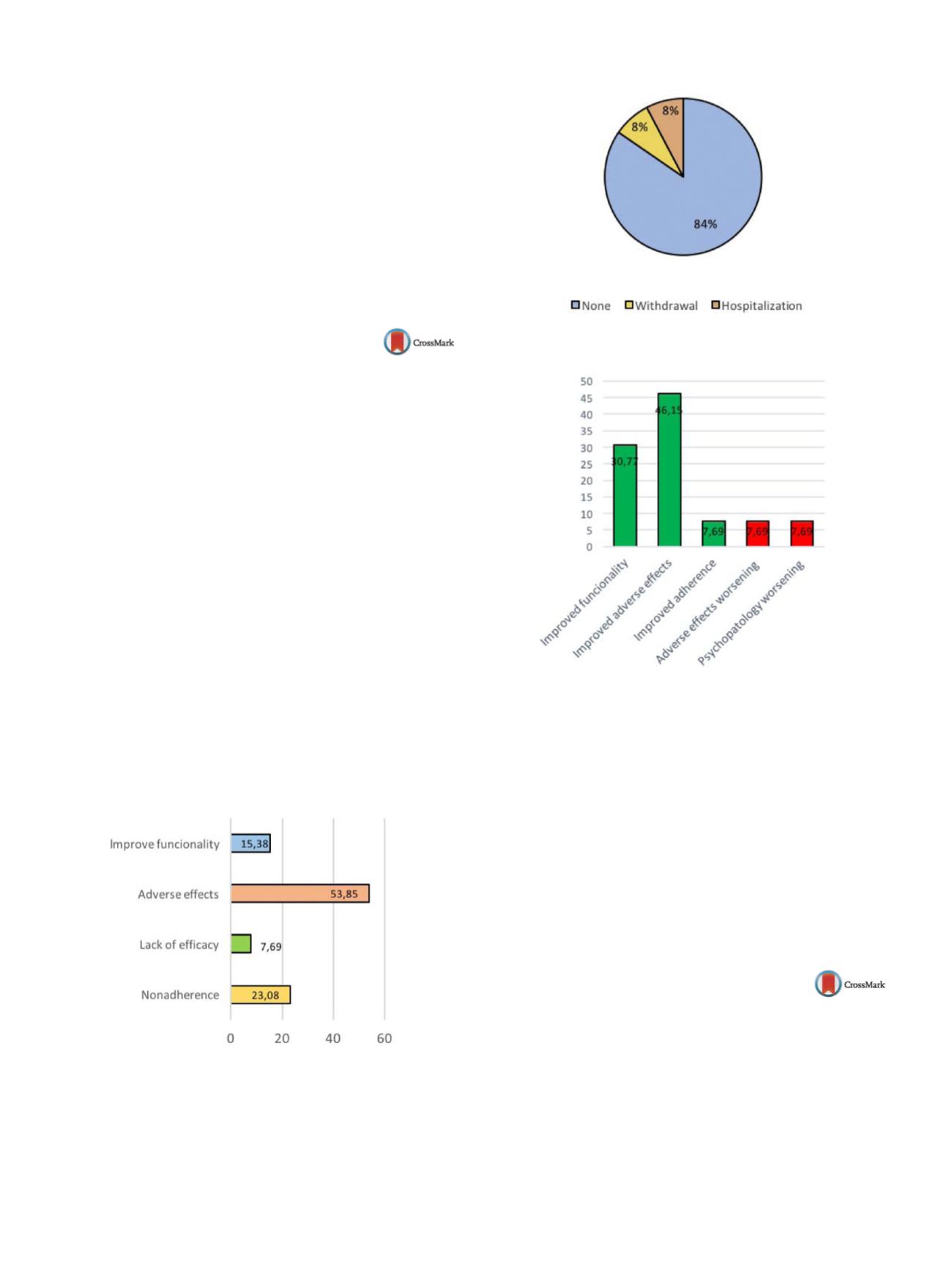
Results
Mean age was 53.69; 53.8% were males and 46.2%
females. The most frequent diagnosis was Schizophrenia and other
chronic psychosis (69.3%). Only 7.7% had co-morbidity with sub-
stance use disorder (cocaine); 61.6% were on previous treatment
with other injectable anti-psychotics; 84,6% of the sample received
AOM as monotherapy. Reasons for switching to AOM are shown on
Fig. 1 . Events during switching are shown on
Fig. 2 . Outcomes with
AOM long-term treatment were positive in 84.61% of cases and are
shown on
Fig. 3 .Conclusions
Switching to AOM could be considered as a good
strategy to improve tolerability, functionality andultimately adher-
ence to treatment in patients in middle age of life with a chronic
psychotic disorder
[2] .Fig. 1
Reasons for switching.
Fig. 2
Events during switching.
Fig. 3
Outcomes with AOM.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
References
[1] Kane J, Peters-Strickland T, Ross A, et al. Aripiprazole once-
monthly in the acute treatment of schizophrenia: findings
from a 12-week, randomized, double-blind, placebo-controlled
study. J Clin Psychiatry 2014;75(11):1254–60.
[2] Fagiolini A, Brugnoli R, Di Sciascio G, et al. Switching
antipsychotic medication to aripiprazole: position paper by
a panel of Italian psychiatrists. Expert Opin Pharmacother
2015;16(5):727–37.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1426EV1097
Clinical vignette – Aripiprazol long
acting injection monotherapy as
long-term treatment for bipolar
disease
C. Solana
∗
, S. Nascimento , M. Duarte , M. Mendes
Centro Hospitalar Psiquiatrico de Lisboa, Psychiatry, Lisboa, Portugal
∗
Corresponding author.
Introduction
Over the last decade a number of effective mainte-
nance treatments for bipolar disorder (BPD) have been developed.
Lithium remains the best-established option, but valproic acid,
lamotrigine, olanzapine, and quetiapine are also effective main-
tenance drugs. However, oral administration contributes to lower
adherence rates with these drugs. In the United States and Europe,


















