
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S710–S771
S763
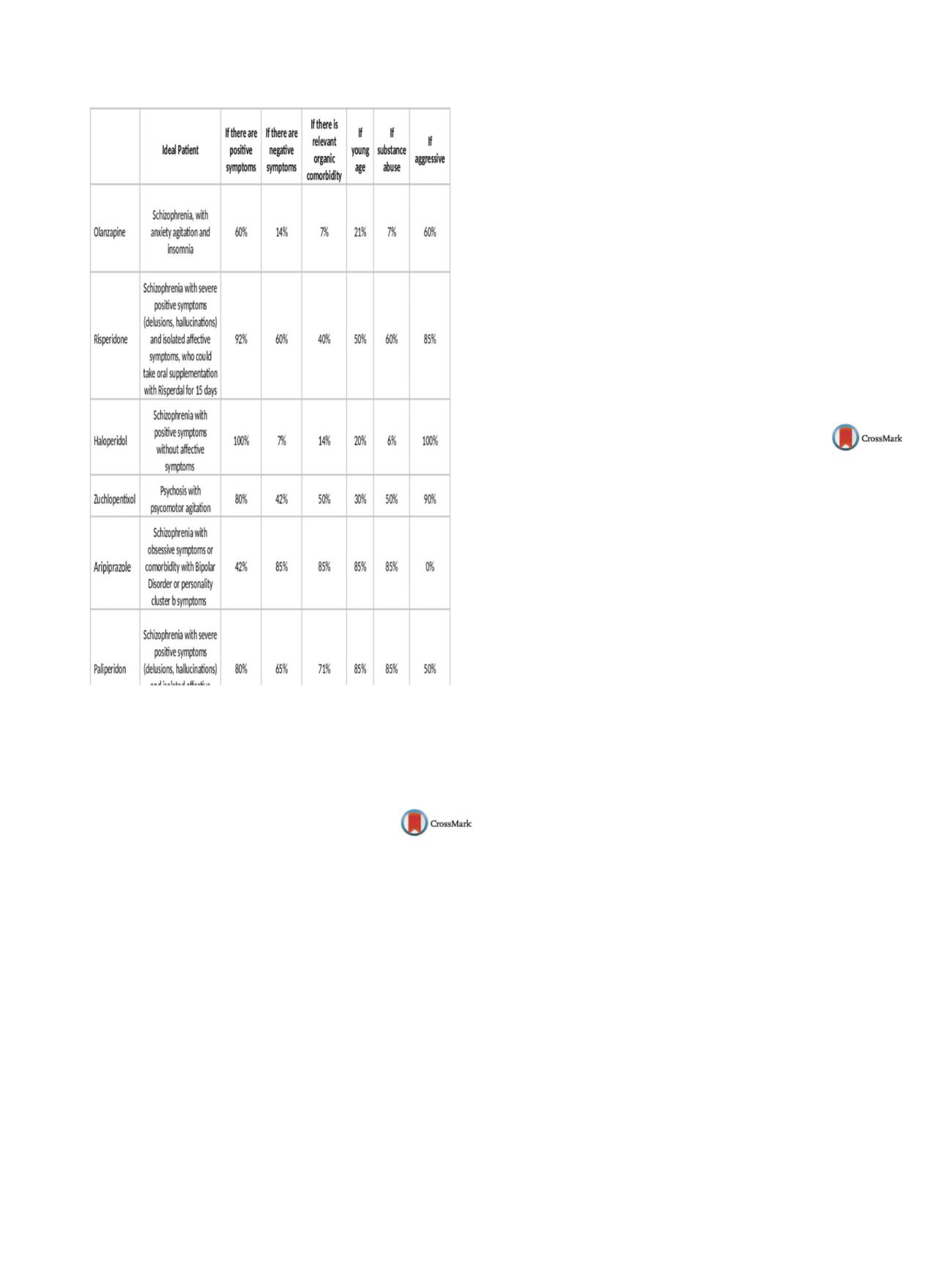
Table 2
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1432EV1103
Genital cenestopathy in psychotic
depression responds to augmentation
with aripiprazole and pregabaline: A
case report
S. ˇCekerinac
1 ,∗
, V. Vukovi´c
21
General Hospital Sremska Mitrovica, General Psychiatry Ward,
Sremska Mitrovica, Serbia
2
Special Hospital for Psychiatric Disorders “Dr Slavoljub Bakalovi´c”,
Acute Psychosis Ward, Vrˇsac, Serbia
∗
Corresponding author.
Introduction
Psychotic depression is a well-known entity, with
recent data confirming the use of antidepressant and anti-psychotic
co-treatment. Psychotic symptoms can be mood incongruent and
present further difficulties for treatment.
Case summary
A 51-year-old female presented to our hospi-
tal, with symptoms of genital cramping, paresthesiae, feelings of
unease in the vulva and depressive mood. In December 2014, the
patient was diagnosed with genital polyps, which were success-
fully removed by curettage. The patient continued feeling various
genital symptoms, which she associated with social and fam-
ily stressors. After short initial outpatient treatment, the patient
was admitted to our ward for complete assessment. Psycholog-
ical assessment revealed psychotic elements, high anxiety and
a passive aggressive personality. Abdominal ultrasound, lumbal
spine radiography, physiatrist exam and computerized tomog-
raphy of the brain showed no abnormalities. The patient was
diagnosed with psychotic depression and referred to further out-
patient treatment. Her drug regimen consisted of venlafaxine,
risperidone, clonazepam and carbamazepine, which led to slight
initial improvement. However, the patient still referred persistent
symptoms as well as sedation as an adverse effect, so risperidone
was switched to aripiprazole, and carbamazepine to pregabaline.
The initiation of this treatment has led to complete withdrawal of
symptoms and the patient has since maintained stable remission.
Conclusion
Aripiprazole is well suited to the female population
because of its lack of hyperprolactinemia, and its combination with
pregabaline may be an option for augmenting treatment in psy-
chotic depression with cenestopathy.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1433EV1104
Hyperprolactinemia and
anti-psychotics: Prevalence and risk
factors
B. Walid
∗
, I. Marrag , R. Ben Soussia , F. Ellouze , M. Nasr
Hospital, Psychiatrie, Mahdia, Tunisia
∗
Corresponding author.
Introduction
Hyperprolactinemia is a frequent side effect
observed in patients treated with anti-psychotic drugs. The fre-
quency of clinical signs usually correlates with elevated serum
prolactin levels.
Objectives
To estimate the prevalence of hyperprolactinemia
among patients treated with a single anti-psychotic and specify
the risk factors for its occurrence.
Methods
Cross-sectional study performed in a period of 6months
in the psychiatric department of Mahdia’s hospital, for all patients
seen in the consultation and treatedwith a single anti-psychotic for
12 weeks, with a stable dose, and meeting the inclusion and exclu-
sion criteria of the study. Prolactin blood tests have been performed
and confirmed by a second one in case of abnormality objectified in
the first lab test results. A magnetic resonance imaging (MRI) was
intended for patients with prolactin levels greater than 150 ng/mL.
Results
Ninety-two patients were gathered. Prevalence of hyper-
prolactinemia was 34.8% of which 7.6% had prolactin levels greater
than 150 ng/mL. Two macroadenomas’ cases were detected. The
analytical study found 7 factors significantly correlatedwith hyper-
prolactinemia, which are: female sex, substance use, the presence
of side effects, prescription of atypical anti-psychotics, the anti-
psychotic treatment prescribed: haloperidol/amisulpride, doses of
anti-psychotic greater than 1000mg equivalent to chlorpromazine
and the combination of psychotropic drugs.
Conclusion
Prolactin blood test should be a systematical analysis
for all patients treated with anti-psychotics, to prevent the short
and long term side effects.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1434

















