
S824
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S772–S846
EV1279
Efficacy of memantine in
schizophrenic patients: A systematic
review
C. Montemitro
∗
, M.C. Spano , M. Lorusso , G. Baroni , G. Di Iorio ,
M. diGiannantonio
Department of Neuroscience, chair of Psychiatry, University “G.
d’Annunzio”, Department of Neuroscience Imaging and Clinical
Science, Chieti, Italy
∗
Corresponding author.
Introduction
Several evidences support the hypothesis that glu-
tamatergic dysfunction may be implicated in the pathogenesis
of schizophrenia and in the last few year great interest has
been focused on the role of the N-methyl-D-aspartate receptor
(NMDAR). Memantine is a noncompetitive NMDARs antagonist,
binds the same site of NMDARs of Mg2+, endogenous blocker of
NMDARs, with moderate affinity, rapid unblocking kinetics and
strong functional voltage-dependency. Memantine does not affect
the physiological activation of NMDARs whereas it blocks the sus-
tained activation under pathological conditions. Preclinical studies
have demonstrated that memantine at high concentrations tar-
gets many receptors, including serotonin, nicotinic acetylcholine,
sigma-1 and serotonin and dopamine receptors.
Objectives
Increasing interest in memantine add-on therapy in
schizophrenic patients with negative and cognitive symptoms may
suggest that memantine could be a new promising treatment in
schizophrenia.
Aims
The aim of this update was to evaluate clinical data about
the memantine effectiveness in schizophrenic patients.
Methods
We searched on PubMed to identify original studies
about the use of memantine in treatment of schizophrenic patients.
The search conducted on June 16th, 2016 yielded 135 records. Neuf
papers met our inclusion criteria.
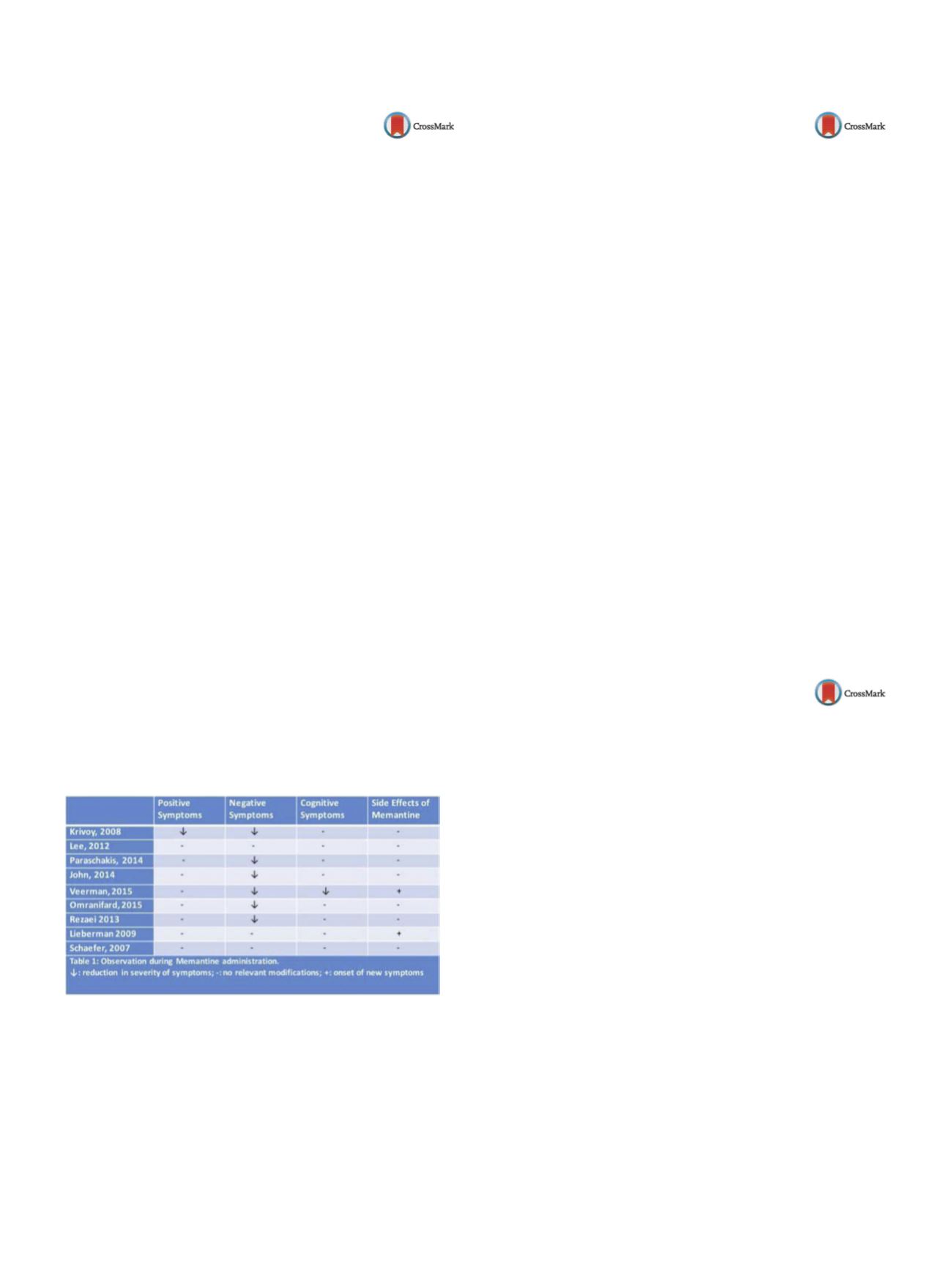
Results
Negative symptoms improved in the large majority of
patients treated, however there is not a clear evidence on cognitive
and positive symptoms
( Table 1 )Conclusions
Memantine therapy in schizophrenic patients has
given unclear results. It seems that memantine improves mainly
negative symptoms, while cognitive and positive symptoms did not
improve significantly. Further trials with a more numerous sample
are required obtain an objective result.
Table 1
Observation during Memantime administration.
↓
: reduction in severity of symptoms; -: no relevant modifica-
tions; +: onset of new symptoms
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1609EV1280
Stressors in patients with
schizoaffective disorder
L. Montes Reula
∗
, H. Saiz García , A. Portilla Fernández
Biomedical Research Center CIB, Psychiatric, Pamplona, Spain
∗
Corresponding author.
Patients with schizoaffective disorder have recurrent episodes of
a mood disorder with severe psychotic symptoms. In many cases,
patients have toxic abuse in some situations that could cause con-
fusion in symptoms and ranking it. It is about a patient diagnosed 5
years ago of schizoaffective disorder with decompensation caused
by leaving medication and drug consumption. A year ago, the
treatment was changed to intramuscular formulation with abil-
ify maintena to ensure compliance and adherence. The patient
continues to consume toxic in weekends, with symptoms of self-
referentiality and suspicion towards their environment. Twoweeks
ago, he was with the girlfriend of a friend and after this event, the
friend has been threatening him. The patient has a state of anxiety
rising, with interpretations and associations delirious about this
friend. He sleeps with a knife in bed if the friend entered his home.
It is a very overwhelmed situation, magnifying and causing severe
impact on their underlying disorder. When the patient is evalu-
ated, it is decided to add treatment with olanzapine a few days to
reduce symptoms and anxiety. Patients withmental disorders have
stressors that cause anxiety like a healthy patient. It is true that the
impact it has on the patients tend to be older and to overvalue the
signs and real situations. In these cases should not be considered a
decompensation and attribute symptoms to lack of efficacy of treat-
ment. In many cases, if we associate a more sedating antipsychotic
profile, they shall reduce symptoms.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1610EV1281
Insight and apathy in patients with
paranoid schizophrenia:
Rehabilitation approaches
O. Papsuev , L. Movina
∗
, M. Minyaycheva , I. Gurovich
Moscow Research Institute of Psychiatry, Outpatient Psychiatry and
Organization of Psychiatric Care, Moscow, Russia
∗
Corresponding author.
Introduction
For many decades, clinicians were very well aware
of lack of insight in patients with paranoid form of schizophrenia.
This group of patients is not only less compliant with pharma-
cotherapy, but also is hard to manage in the rehabilitation setting.
This dictates the necessity to develop special approaches to this
group of patients, based on clinical data.
Method
Fifty patients with schizophrenia spectrum disorder
were randomly recruited to be assessed by PANSS scale and Apa-
thy Evaluation Scale (AES), which was introduced both by trained
clinicians (C) and as a self-assessment measure (S). Demographic
data was collected along with clinical description on prevailing
symptoms during acute phase.
Results
While AES-C scoreswere verywell correlatedwith PANSS
motivation subscale, AES-S scores showed prominent discrepan-
cies both with PANSS items and AES-C version. Lower scores on
AES-S were also associated with paranoid schizophrenia and pre-
vailing delusional symptoms in acute phase. As well AES-C/AES-S
ratio also correlated with paranoid form and delusional symptoms
in manifest psychoses.
Discussion
Patients with paranoid schizophrenia not only lack
insight into positive symptoms, but tend to underestimate their
negative symptoms such as motivation and apathy. Clinically, this
can be described by overestimated strengths, overstated expecta-
tions, exaggerated hopes, mistakenly overrated beliefs. But when


















