
S354
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S303–S364
they place on patients, may increase the rate of incidents within
the hospital. Despite comparable rates on admission, MI rehabili-
tation wards have far fewer incidents than PD rehab wards, which
may reflect the more intractable nature of PD versus MI. More work
is required to confirm these findings.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.335EW0722
An analysis of emergency leaves of
absence from a United Kingdom high
secure psychiatric hospital with a
view to identifying ways to reduce
their number
H. Blott
∗
, C. Gordon , J. Bickford , C. Ross
West London mental health trust, forensic psychiatry, London, United
Kingdom
∗
Corresponding author.
Introduction
Emergency leaves of absence (ELOAs) from high
secure psychiatric care are both costly and increase the risk posed
to staff, patients and the general public. ELOAs were analysed to
identify whether greater on-site physical health provision could
reduce their number, and quantify the potential financial saving to
the trust to do so.
Method
All ELOAs from Broadmoor hospital between
15.5.15–14.11.15 were assessed by a team of psychiatrists
and a GP to identify whether they were “avoidable”, “unavoidable”
or “potentially avoidable” if measures were taken. For the “poten-
tially avoidable” group, we then calculated the staffing cost of
these LoAs to help ascertain whether these measures would be
cost effective.
Results
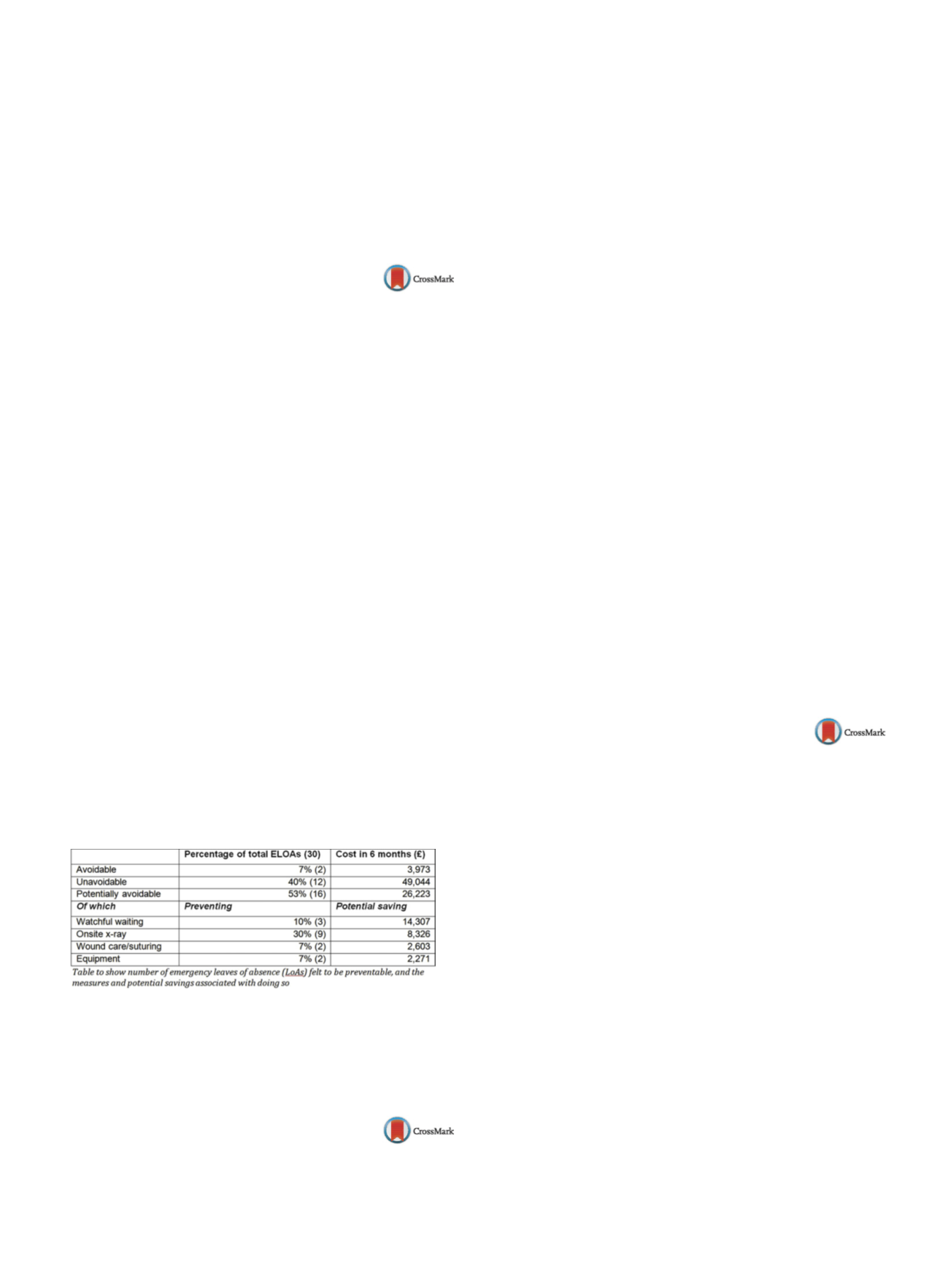
There were 30 ELOAs during the period assessed, costing
£
79,240
( Table 1 ).The table also shows which additional on-site
services or training may have prevented these ELOAs, and the cost
saving to the trust if they had.
Conclusions
The number of ELOAs from the hospital could be
reduced by increased on-site physical health provision and trai-
ning. This would improve the quality of care patients receive, as
well as reducing both the cost to the trust and the risk posed to
staff, patients and the general public. We must also consider the
large potential cost and risks associated with a patient absconding
from an ELOA.
Table 1
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.336EW0723
The relationship between grief
process and attachment styles in the
cases with the treatment of
complicated grief: A prospective study
H.P. Caglar Nazali
1 ,∗
, E .A. Yildirim
21
Baltalimani Metin Sabanci bone and joint diseases education and
research hospita, psychiatry, Istanbul, Turkey
2
Bakirkoy research and training for psychiatry neurology
neurosurgery, psychiatry, Istanbul, Turkey
∗
Corresponding author.
The attachment style is one of the significant factors affecting the
grief process and complicated grief. This study aims to research
the relation between the factors determining the sociodemogra-
phic features, the reactions of grief, the suicidal behaviour and the
grief process on the patients who are followed and treated with
the complicated grief diagnosis and the features of attachment.
The study includes 45 patients directed to a therapy unit and meet
the criterions of complicated grief diagnosis. 33 of those patients
have completed their treatment. Sociodemographic and clinical
data form applied to the patients at the beginning, to evaluate
for comorbid psychiatric disorders structured clinical interview
for DSM-IV axis I disorders, adult attachment style questionnaire
(AASQ), grief scale, hamilton rating scale for depression (HDRS), sui-
cide behaviors questionnaire (SBQ), suicide probability scale (SPS),
experiences in close relationships inventory (ECRI) are applied on
the participants and compared the results of the scales prior to and
following the treatment. In the dimensional evaluation of attach-
ment, ECRI avoidance score is high over the patients diagnosedwith
comorbid psychiatric disorders with complicated grief. During the
first application of the treatment, while evaluating the attachment
categorically, in the complicated grief patients attached with avoi-
dance grief scale, behavioural base scale and SPS negative self base
scale are higher compared to the group whose HDRS scores atta-
ched with secure. The results show that in complicated grief cases
the avoidance attachment is both dimensionally and categorically
relatedwith the strength of grief reaction and additional psychiatric
problems.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.337EW0724
Cognitive disturbances and mood
disorders in ischemic stroke
E.I. Davidescu
∗
, D.A. Sasu , I. Buraga
UMF Carol Davila, neurology Colentina clinical hospital, Bucharest,
Romania
∗
Corresponding author.
Introduction
Ischemic stroke is in increasing incidence, so that
long term sequels are of great importance for management of qua-
lity of life and economics issues.
Objectives
To determine risk factors associated with cognitive
disturbances, after ischemic stroke.
Aims
Assessment of social and medical risk factors in outcome of
cognitive disturbances.
Methods
During 6 months, 268 patients with antecedents of
ischemic stroke and associated cognitive disturbances installed in
first year after major stroke, were assessed in neurology depart-
ment. We performed neuropsychological tests as mini mental state
examination, sunderland clock test and beck depression inventory.
Patients and caregivers were also assessed for quality of life. 53%
were males, from urban areas (69%) and mean age was 72.2 years.
Results
We found risk factors as hypertension (88%), dyslipide-
mia (63%), diabetes mellitus (22%), atrial fibrillation (11%), smoking
(35%) and drinking (55%). According to DSM-5 criteria, 62.5% of
our lot had major cognitive disorder and 37.5% had a minor one;
most of the patients with major dysfunction had ischemia in left
middle cerebral artery (31.71%) associated with language defi-
cits and executive dysfunctions, and on the second place was the
vertebro-basilar localization of stroke (29.86%). Ischemia in right
middle cerebral artery was present only in 20.52% of the lot. 27%


















