
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S303–S364
S347
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.316EW0703
The squeezing snake, a psychiatric
presentation of epilepsy: A case report
M. Mangas
∗
, L. Bravo , Y. Martins , A. Matos Pires
Hospital José-Joaquim Fernandes, mental health and psychiatric
service, Beja, Portugal
∗
Corresponding author.
Introduction
Epilepsy is considered a complex neurological
disorder with a great variety of clinical presentations that can
resemble psychiatric disorders.
Objectives
Disclose an unusual clinical case with psychiatric
symptoms as the presentation of epilepsy.
Methods
Psychiatric assessments and retrospective reviewof the
clinical file and literature research.
Results
A 40-years-old Romanian woman presented to the psy-
chiatry outpatient service with a history of persistent depressive
mood and disturbed sleep for the past 3 years, complaining of a
feeling that she described as “a snake squeezing around her body,
starting in her left leg and spreading to the rest of her body up
to the neck” associated with a sense of pins and needles, occurring
during night time. She attended general practice, neurosurgery and
psychiatry appointments. Her medical history included “gastritis”
and lower left leg fracture and a pituitary microadenoma revea-
led in brain CT-scan. Blood work, including endocrine tests and
brain-MRI were normal. Her symptoms initially led to diagnosis
of: anxiety, somatization, Ekbom syndrome and depression. She
was treated with antidepressives, antipsychotics and anxiolytics,
without response. After careful reconstruction of the clinical his-
tory and further analyses of her complaints, the diagnosis of focal
sensory jacksonian seizure was made. Levetiracetam introduction
led to symptomatic remission.
Conclusion
Epilepsy includes a variety of neuropsychiatric symp-
toms. This case illustrates that epileptic patients may experience
non-convulsive seizures that might be mistaken as primary psy-
chiatric disorders. Neurologists and psychiatrists must be aware
of this varied presentation while obtaining the medical history in
order to investigate and manage this patient effectively.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.317EW0704
A case of neurosyphilis in a patient
presenting with bipolar mixed
episode suggestive symptoms
M. Martins , R. Fernandes
∗
Centro hospitalar Psiquiátrico de Lisboa, psiquiatria geral e
transcultural, Lisbon, Portugal
∗
Corresponding author.
Introduction
Syphilis is a sexually transmitted disease caused by
Treponema pallidum
. Early invasion of the central nervous system
might occur early in the course of the disease. Clinical manifes-
tations may include acute meningeal syphilis, meningovascular
syphilis, paretic neurosyphilis and tabetic neurosyphilis. Psychia-
tric symptoms are often the presenting symptoms of this illness
and the correct diagnosis involves both a high degree of suspicion
and adequate diagnostic tests.
Objectives
The authors report a case of a patient, with no previous
history ofmental illness, initially admitted in a psychiatric unit with
a clinical picture suggestive of a mixed bipolar disorder episode
who has been diagnosed with neurosyphilis a year after.
Methods
Review of clinical records and complementary exams.
Results
By the first admission, the patient presented with
depressed and irritable mood, emotional lability, aggressiveness,
grandiose and racing thoughts. Upon discharge, he was diagnosed
with bipolar disorder and referred to ambulatory unit. The follo-
wing year he starts presenting cognitive deficits and a progressive
loss of autonomy in daily living activities, being referred to neuro-
logy evaluation. A year after the first admission, he is admitted in a
neurology unit and diagnosed with neurosyphilis.
Conclusions
Current prevalence of symptomatic neurosyphilis in
Western Europe is unknown. Atypical cases presenting with hete-
rogeneous psychiatric and neurologic symptoms, with no previous
history of mental illness, should raise a high index of clinical sus-
picion, since consequences for the patient’s health might be severe
if not properly diagnosed and treated.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.02.318EW0705
Reduced left frontal GABA in
ultra-high risk of psychosis patients.
1H MRS study
P. Menshchikov
∗
, T. Akhadov , N. Semenova
Scientific research institute of urgent children’s surgery and trauma,
radiology, Moscow, Russia
∗
Corresponding author.
Introduction
Some previous findings indicate participation dis-
turbance of balance between excitatory (GABA) and inhibitory (Glu)
neurotransmitters in pathogenesis of schizophrenia. The aim of
this study was to evaluate GABA and GLX levels in the brain of
medicated UHR subjects.
Objectives
Twenty-one (18–25 years, mean = 19.4, SD = 3.5) right-
handed medicated UHR men and 26 (18–25 years, mean = 19.8,
SD = 2.2) mentally healthy volunteers participated in this study. The
patientswere included in theUHR group in accordancewith criteria
of prodromal states.
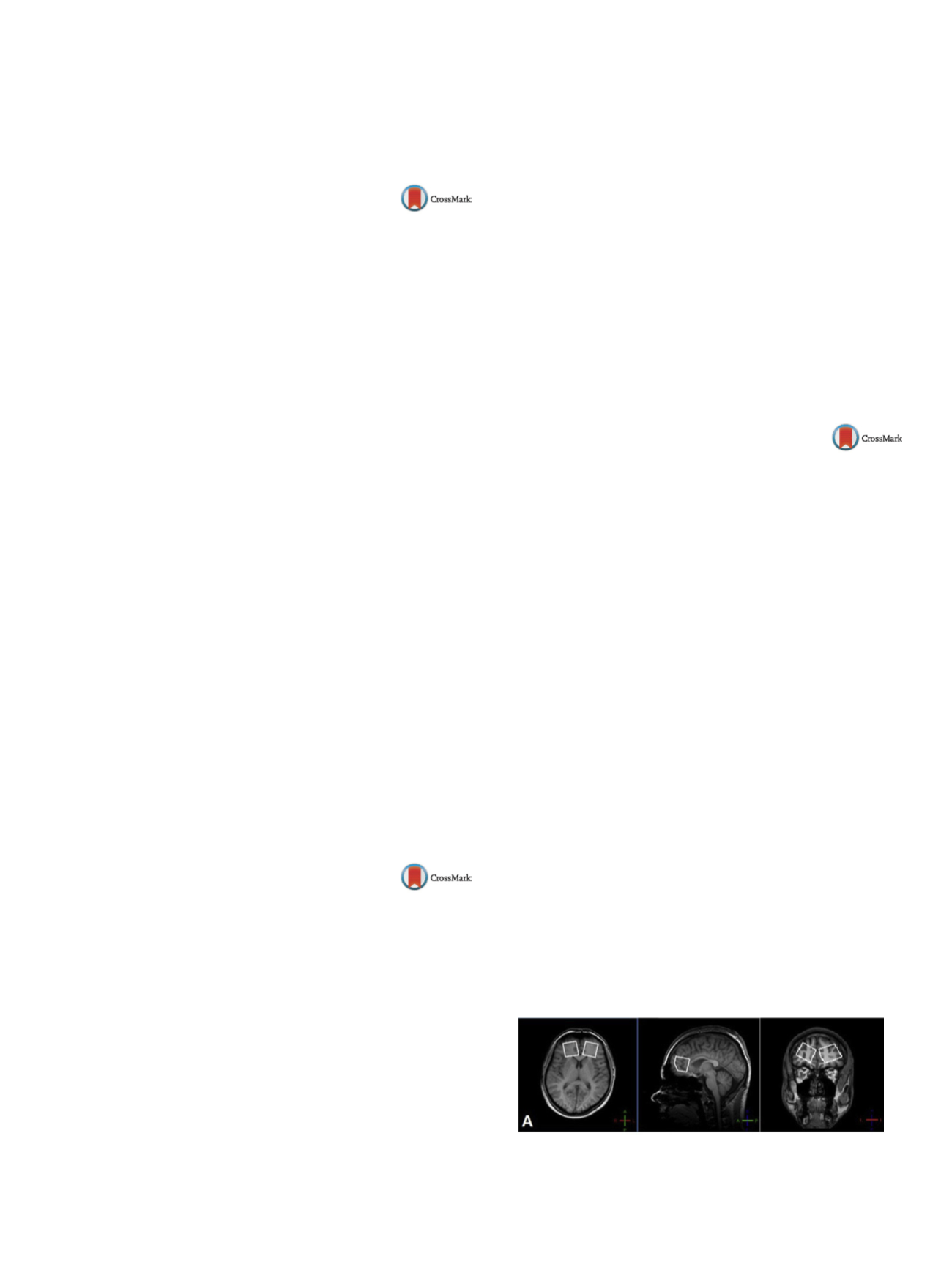
Methods
1H MRS (MEGA-PRESS pulse sequence [Mescher, NMR
Biomed 1998;11:266]) was used for GABA and GLX detection.
Volumes of interest in size of 30
×
30
×
30mm were placed in the
left and right frontal lobes in the areas of the anterior cingulate
cortex (ACC)
( Fig. 1 ).Results
The main effects on the GABA/Cr (
t
[45] = 4.17,
P
< 0.01)
( Fig. 2 A) and GABA/GLX (
t
[45] = 2.84,
P
< 0.01)
( Fig. 2 B), were found
in the left ACC (t[45] = 4.17,
P
< 0.01), with the patients having lower
GABA/Cr and GABA/GLX ratios as compared to the control group.
Also significant negative correlation (
r
=
−
0.49,
P
= 0.04) between
GABA/Cr in the right ACC and the current daily dosage of antipsy-
chotic medication in CPZ-Eq was found
( Fig. 3 ).Conclusion
This study reveals for the first time a significant
reduction of (GABA) (25%) and GABA/GLX ratio (20%) in left AC of
UHR subjects. According to (de la Fuente-Sandoval, Int J Neuropsy-
chopharmacol 2015;19[3]) and association of (GABA) with daily
dosage of medication found, this reduction may be caused by the
antipsichotic treatment.
Fig. 1
1H MRS VOI localizations.


















