
25th European Congress of Psychiatry / European Psychiatry 41S (2017) S772–S846
S805
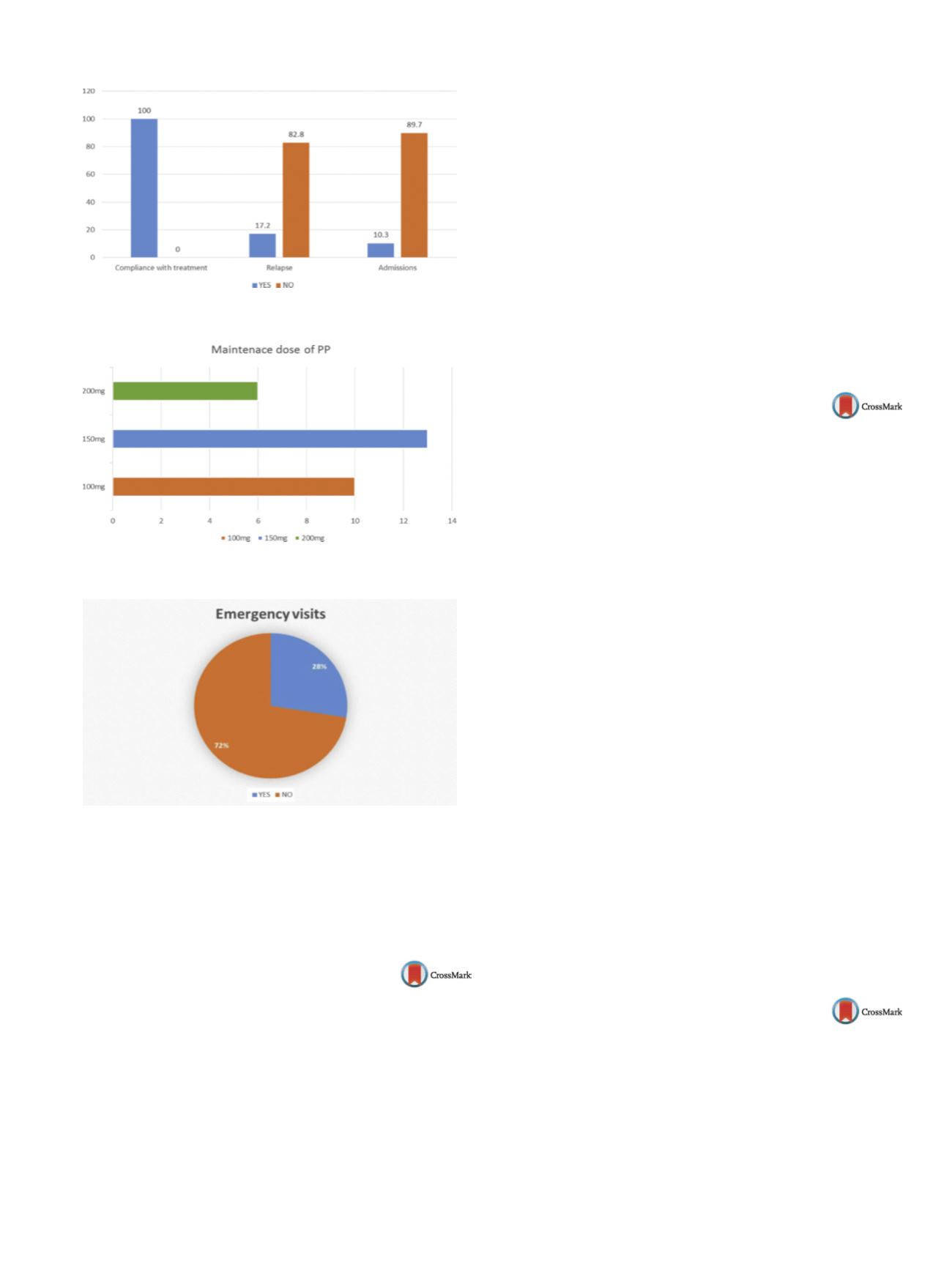
Fig. 1
Fig. 2
Fig. 3
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1556EV1227
Vitamin B12 deficiency induced
psychosis – a case report
A.R. Carvalho
∗
, S. Vacas , C. Klut
Servic¸ o de Psiquiatria- Hospital Beatriz Ângelo, Departamento de
Psiquiatria e Saúde Mental, Hospital Beatriz Ângelo, Lisboa, Portugal
∗
Corresponding author.
Vitamin B12 is one of the most essential vitamins affecting various
systems of the body. Cases of neuropsychiatry disorders due to its
deficiency are more common in elderly patients with prevalence of
10–20%. The most common psychiatry symptoms reported in the
literature associated with vitamin B12 deficiency was depression,
mania, psychotic symptoms, cognitive impairment and delirium.
Here, we report a case of vitamin B12 deficiency in a 52-year-
old male who presented with psychotic features: persecutory
delusions, tactile and auditory hallucinations. Patient had neither
recorded psychiatry history nor any drug abuse. Medical history
includes hypertension, diabetesmellitus and glaucoma. The patient
was not a vegetarian. All relevant laboratory evaluations and head
CT were normal except vitamin B12. The patient was treated with
antipsychotics (risperidone 3mg/day) and intramuscular vitamin
B12. One week after, there was total remission of psychotic symp-
toms. In the follow-up during the next four months, psychiatry
symptoms did not recur at any time. This case reports a rare case
of vitamin B12 deficiency induced psychosis. Although there was
concurrent administration of an antipsychotic along with vitamin
B12, it underlines the importation of evaluation of vitamin B12 and
other potential reversible causes of psychosis.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1557EV1228
QTc interval in patients diagnosed
with schizophrenia receiving different
defined daily dose (DDD) of
antipsychotics
T. Christensen
1 ,∗
, R. Møller Jeppesen
21
Aarhus University Hospital Risskov Denmark, Department of
Psychiatry, København Ø, Denmark
2
Aarhus University Hospital Risskov Denmark, Department of
psychiatry, Aarhus, Denmark
∗
Corresponding author.
Introduction
Both 1st and 2nd generation of antipsychotics are
associated with prolonged QTc interval. Prolonged QTc can lead
to ventricular tachycardia and Torsade’s de pointes, ultimatime
resulting to cardiac arrest and sudden death. ProlongedQTc interval
due to increased DDD has not yet been investigated.
Objective
To investigate whether increased DDD of antipsy-
chotics, causes further prolonged QTc, by patients diagnosed with
schizophrenia.
Aims
To learnmore about antipsychotics impact on theQTc inter-
val in patients diagnosed with schizophrenia.
Methods
An observational study of unselected patients diag-
nosed with schizophrenia. Enrolled from January 2013 through
March 2015 with follow-up until June 2015 in the region of cen-
tral Denmark. Data was collected from ECG records and patient
journals.
Result
ECGs were available in 58 patients. We observed no rela-
tion between increased DDD of antipsychotics and prolonged QTc.
There were no differences in average QTc interval for the whole
sample of patients receiving different DDD of antipsychotics.
Conclusion
We do not recommend increased attention to
patients treated with higher DDD of antipsychotics.
Disclosure of interest
The authors have not supplied their decla-
ration of competing interest.
http://dx.doi.org/10.1016/j.eurpsy.2017.01.1558EV1229
Normalization of mortality rate and
life expectancy in schizophrenia:
Challenges and options
D. Cohen
Mental Health Care Organization Noord-Holland North, Community
Mental Health, Heerhugowaard, Netherlands
Studies of mortality-rates and life expectancy in schizophrenia
have consistently shown that the standardized mortality rate
(SMR) are raised compared to the general population. In a meta-
analysis (2007) of 38 studies with 22,296 deaths, all cause SMR
was 2.98. SMR in a French cohort study (2009) in 3470 patients


















